
Adenocarcinoma of the bladder: a case report
Highlight box
Key findings
• We report a rare case of adenocarcinoma of the urinary bladder associated with intestinal metaplasia and cystitis glandularis of the urinary bladder treated by robot-assisted radical cystectomy. The patient was free from recurrence 1 year after the surgery.
What is known and what is new?
• Adenocarcinoma of the urinary bladder is rare and has a poor prognosis. The main treatment option is radical cystectomy.
• We present the first case report of adenocarcinoma of the urinary bladder treated by robot-assisted radical cystectomy.
What is the implication, and what should change now?
• The patient diagnosed with adenocarcinoma of the urinary bladder underwent robot-assisted radical cystectomy and was free from recurrence 1 year after the surgery. Accumulation of similar case reports would improve the treatment of patients with bladder adenocarcinoma.
Introduction
Background
Adenocarcinoma of the urinary bladder is a rare malignant disease that accounts for 0.5–2.0% of all cases of bladder cancer (1). Possible risk factors for bladder adenocarcinoma include schistosomiasis, chronic inflammation, urinary obstruction, cystocele, and endometriosis (2). Adenocarcinoma of the bladder largely arises from the trigon or the posterior wall of the bladder. The tumor may appear as a papillary, sessile, or ulcerous lesion. Notably, the prognosis of bladder adenocarcinoma is poor, with reported overall 2-, 5-, and 10-year survival rates of 54.8%, 36.1%, and 25.4%, respectively (3).
Various benign glandular lesions, including cystitis glandularis, should be considered in the differential diagnosis of bladder adenocarcinoma (4-7). Cystitis glandularis, a relatively rare condition of proliferative cystitis, is generally classified into two categories: (I) usual/typical and (II) intestinal (also known as intestinal metaplasia) (6). The presence of extracellular mucin secreted by goblet cells confirms the differential diagnosis of endocervicosis, primary adenocarcinoma, or urachal adenocarcinoma (5).
Rationale and knowledge gap
The prognosis of bladder adenocarcinoma is poor, with reported overall 2-, 5-, and 10-year survival rates of 54.8%, 36.1%, and 25.4%, respectively (3). Optimal treatment for bladder adenocarcinoma remains to be established.
Objective
We report a case of adenocarcinoma, not otherwise specified (NOS), associated with intestinal metaplasia and cystitis glandularis of the urinary bladder treated by robot-assisted radical cystectomy (RARC). This case is presented in accordance with the CARE reporting checklist (available at https://asj.amegroups.com/article/view/10.21037/asj-23-3/rc).
Case presentation
A 43-year-old man was referred to the urology department of another hospital with a bladder tumor that was incidentally detected during ultrasonography. Cystoscopy revealed a follicular tumor in the trigon of the urinary bladder, but the orifices were not detectable (Figure 1A). The patient underwent a transurethral resection of the bladder tumor. Pathological examination revealed adenocarcinoma, NOS, associated with intestinal metaplasia and cystitis glandularis.
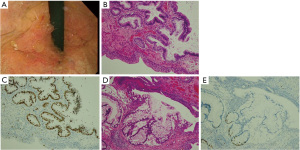
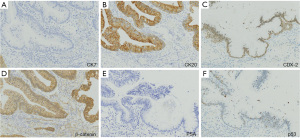
Most parts of the specimen exhibited intestinal metaplasia and cystitis glandularis. Microscopically, a large and clear nucleus was observed in some of the tumor cells containing the gland ducts. The Ki-67 positivity rate was higher in these regions than in the other regions, and breakdown of the gland ducts and mucus leakage into the proper mucus membrane suggested tumor invasion into the proper mucus membrane (pT1) (Figure 1B-1E). No muscular invasion or vascular infiltration was observed. Immunohistochemical (IHC) staining showed cytokeratin (CK) 7(−), CK20(+), Caudal type homeobox 2 (CDX-2) (+), and no nuclear localization of β-catenin (Figure 2A-2D). The specimen was negative for prostate-specific antigen (Figure 2E). P53 testing showed a wild pattern (Figure 2F). The final pathological diagnosis was adenocarcinoma NOS associated with intestinal metaplasia and cystitis glandularis. No evidence of urothelial carcinoma was observed in any specimen.
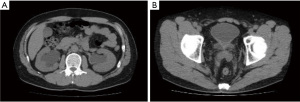
The patient underwent repeated transurethral resection of the bladder tumor, and no residual tumor was found. However, the trigon of the urinary bladder was still inflamed. Computed tomography revealed severe bilateral hydronephrosis, but no other tumors were detected (Figure 3). Gastroscopy and colonoscopy revealed no other tumors. The urine cytology was negative for malignancy throughout the treatment period.
Although the histological examination of the second transurethral resection was negative for cancer, because of the severe hydronephrosis and the tumor’s possible aggressive behavior, the patient underwent RARC with total intracorporeal urinary diversion (ileal neobladder). Pathological examination revealed no residual tumor (pT0). The patient had the periodic cystoscopy, urine cytology, and computed tomography and was free from recurrence 1 year after the surgery.
All procedures performed in this study were in accordance with the ethical standards of the institutional and/or national research committee(s) and with the Helsinki Declaration (as revised in 2013). Written informed consent was obtained from the patient for publication of this case report and accompanying images. A copy of the written consent is available for review by the editorial office of this journal.
Discussion
Key findings
Here, we report a case of bladder adenocarcinoma associated with intestinal metaplasia and cystitis glandularis treated with robot-assisted radical cystectomy.
Strengths and limitations
This is the first case of bladder adenocarcinoma treated by RARC. The patient is free from recurrence 1 year after surgery. The limitation is that this is a single case report.
Comparison with similar researches
The differential diagnosis of adenocarcinoma from intestinal metaplasia and cystitis glandularis is difficult but clinically important. Intestinal metaplasia may demonstrate mucus extravasation, which can be mistaken for invasive adenocarcinomas. Another possible finding that could mistakenly suggest adenocarcinoma is the presence of benign intestinal metaplasia glands in the muscularis propria or thick muscle bundles (8). In our case, extensive mucus extravasation was found in much of the specimen.
Whether intestinal metaplasia and cystitis glandularis are precancerous remains controversial (9-11). While one retrospective study found no evidence of mucinous metaplasia increasing the future risk of malignancy, others reported the transition from mucinous metaplasia to adenocarcinoma (11).
Explanations of findings
A thorough microscopic examination revealed a 3-mm region that was ultimately diagnosed as adenocarcinoma. IHC examination confirmed the diagnosis of adenocarcinoma. Adenocarcinoma of the bladder reportedly expresses Caudal type homeobox 2 (CDX-2), Carcinoembryonic antigen (CEA), Mucin (MUC)-1, MUC-2, and MUC-3, similar to colonic adenocarcinoma (12). In contrast, bladder adenocarcinoma is positive for CK7 (33.3%) and CK20 (100%), whereas colonic adenocarcinoma is positive for CK20 (100%) but not CK7 (8.3%) (13). Strong nuclear and cytoplasmic-membranous staining of β-catenin was observed in 75% of the metastatic colonic adenocarcinoma cases versus only 16.7% of the primary bladder adenocarcinoma cases (13). Ki-67 is a nuclear protein associated with cellular proliferation and correlated with the clinical course of several cancer types, including bladder cancer (14). A recent systematic review and meta-analysis reported significant correlations between high Ki-67 expression and survival outcomes in European-American but not Asian patients (14).
Considering the severe hydronephrosis and poor prognosis of bladder adenocarcinoma, our patient selected to undergo radical cystectomy.
Implications and actions needed
Although robot-assisted radical cystectomy has been replacing open or laparoscopic radical cystectomy, there are some reports on atypical recurrence of bladder cancer after RARC (15). Surgical indication should be limited to tumors at early stages.
As this is a single case report, accumulation of similar case reports would improve the treatment of patients with bladder adenocarcinoma.
Conclusions
Herein, we report a rare case of bladder adenocarcinoma associated with intestinal metaplasia and cystitis glandularis. The patient underwent Robot-assisted radical cystectomy because of the severe hydronephrosis and poor prognosis of bladder adenocarcinoma and had a favorable outcome.
Acknowledgments
The authors thank the patient for participating in this case report.
Funding: None.
Footnote
Reporting Checklist: The authors have completed the CARE reporting checklist. Available at https://asj.amegroups.com/article/view/10.21037/asj-23-3/rc
Peer Review File: Available at https://asj.amegroups.com/article/view/10.21037/asj-23-3/prf
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at https://asj.amegroups.com/article/view/10.21037/asj-23-3/coif). MN serves as an unpaid editorial board member of AME Surgical Journal from January 2023 to December 2024. The other authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. All procedures performed in this study were in accordance with the ethical standards of the institutional and/or national research committee(s) and with the Helsinki Declaration (as revised in 2013). Written informed consent was obtained from the patient for publication of this case report and accompanying images. A copy of the written consent is available for review by the editorial office of this journal.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Dadhania V, Czerniak B, Guo CC. Adenocarcinoma of the urinary bladder. Am J Clin Exp Urol 2015;3:51-63. [PubMed]
- Montironi R, Lopez-Beltran A, Scarpelli M, et al. 2004 World Health Organization classification of the noninvasive urothelial neoplasms: inherent problems and clinical reflections. Eur Urol Suppl 2009;8:453-7. [Crossref]
- Natale C, Leinwand GZ, Chiang J, et al. Reviewing the Demographic, Prognostic, and Treatment Factors of Primary Adenocarcinoma of the Bladder: A SEER Population-based Study. Clin Genitourin Cancer 2019;17:380-8. [Crossref] [PubMed]
- Williamson SR, Lopez-Beltran A, Montironi R, et al. Glandular lesions of the urinary bladder:clinical significance and differential diagnosis. Histopathology 2011;58:811-34. [Crossref] [PubMed]
- Young RH, Bostwick DG. Florid cystitis glandularis of intestinal type with mucin extravasation: a mimic of adenocarcinoma. Am J Surg Pathol 1996;20:1462-8. [Crossref] [PubMed]
- Sung MT, Lopez-Beltran A, Eble JN, et al. Divergent pathway of intestinal metaplasia and cystitis glandularis of the urinary bladder. Mod Pathol 2006;19:1395-401. [Crossref] [PubMed]
- Morton MJ, Zhang S, Lopez-Beltran A, et al. Telomere shortening and chromosomal abnormalities in intestinal metaplasia of the urinary bladder. Clin Cancer Res 2007;13:6232-6. [Crossref] [PubMed]
- Kryvenko ON, Epstein JI. Mimickers of urothelial neoplasia. Ann Diagn Pathol 2019;38:11-9. [Crossref] [PubMed]
- Smith AK, Hansel DE, Jones JS. Role of cystitis cystica et glandularis and intestinal metaplasia in development of bladder carcinoma. Urology 2008;71:915-8. [Crossref] [PubMed]
- Agrawal A, Kumar D, Jha AA, et al. Incidence of adenocarcinoma bladder in patients with cystitis cystica et glandularis: A retrospective study. Indian J Urol 2020;36:297-302. [Crossref] [PubMed]
- Zhang BY, Aguilar J, Yang M, et al. Mucinous metaplasia in urothelial tract may be the precancerous lesion of mucinous adenocarcinoma: report of two cases and review of literature. Int J Clin Exp Med 2014;7:285-9. [PubMed]
- Sigalas K, Tyritzis SI, Trigka E, et al. A male presenting with a primary mucinous bladder carcinoma: a case report. Cases J 2010;3:49. [Crossref] [PubMed]
- Roy S, Smith MA, Cieply KM, et al. Primary bladder adenocarcinoma versus metastatic colorectal adenocarcinoma: a persisting diagnostic challenge. Diagn Pathol 2012;7:151. [Crossref] [PubMed]
- Tian Y, Ma Z, Chen Z, et al. Clinicopathological and Prognostic Value of Ki-67 Expression in Bladder Cancer: A Systematic Review and Meta-Analysis. PLoS One 2016;11:e0158891. [Crossref] [PubMed]
- Mantica G, Smelzo S, Ambrosini F, et al. Port-site metastasis and atypical recurrences after robotic-assisted radical cystectomy (RARC): an updated comprehensive and systematic review of current evidences. J Robot Surg 2020;14:805-12. [Crossref] [PubMed]
Cite this article as: Izumi T, Nakamura M, Tsuru I, Naito A, Satoh K, Suzuki M, Kume H, Shiga Y. Adenocarcinoma of the bladder: a case report. AME Surg J 2023;3:48.


