
Transmanubrial approach with thoracoscopic surgery for bilateral lung cancer: a case report
Introduction
Selecting an appropriate surgical approach for superior sulcus tumors (SST) is sometimes difficult owing to the anatomy of the region where these tumors appear. The transmanubrial approach (TMA) is useful for anterior SST because it enables good visualization of the major cervicothoracic vessels such as the subclavian vein and artery.
Previous reports have described video-assisted one-sided pulmonary resection combined with TMA for minimally invasive resection (1,2). In this report, we discuss the case of a patient with bilateral lung apex high-grade tumors, which were completely resected using video-assisted pulmonary right upper lobectomy combined with TMA. We also performed partial resection of the left upper portion of the lung using video-assisted thoracoscopic surgery (VATS) with only one postural change. This is the first report of video-assisted bilateral pulmonary resection combined with TMA. We present the following case in accordance with the CARE reporting checklist (available at https://asj.amegroups.com/article/view/10.21037/asj-21-13/rc).
Case presentation
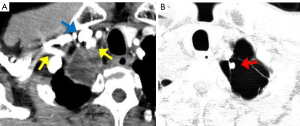
A 68-year-old man with bilateral lung apex tumors was referred to Suwa Red Cross Hospital. The patient was asymptomatic and a chest computed tomography revealed a 40 mm×30 mm solid tumor located in the right lung apex and adjacent to the right subclavian vessels (Figure 1A) as well as a 10-mm solid tumor located in the left upper lobe of the lung, arising from the bulla wall (Figure 1B). Both tumors showed strong uptake of 18F-Fluorodeoxyglucose positron emission tomography. These tumors were suspected to be synchronous primary lung cancer (cT3N0M0 and cT1aN0M0). The possibility of metastasis of the right lung tumor could not be ruled out for the left lung tumor, therefore, we decided to perform left lung partial resection at the same time for diagnostic purposes.
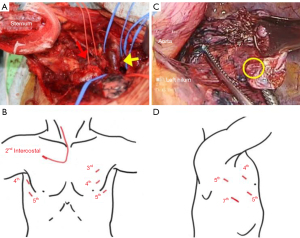
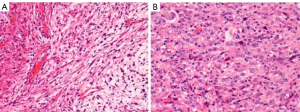
Prior to the start of surgery, the patient was laid in the supine position. The surgery commenced with thoracoscopy to examine the right thoracoscopic cavity and evaluate tumor resectability through 3 ports—one at the second intercostal space on the midclavicular line and two others at the fourth and fifth intercostal space on the anterior axillary line. Since it was judged that the right lung apex tumor could not be detached from the chest wall due to strong adhesion, we proceeded with the TMA. An incision was made along the anterior border of the right sternocleidomastoid muscle and extended parallel to the second intercostal space including the port that was just created. To preserve the sternoclavicular joint, an L-shaped sternal incision was made to reach the first intercostal space. The first costal cartilage was resected near the sternum, and the costoclavicular ligament was dissected behind the clavicle, and a good field of view could then be obtained by raising the clavicle using a traction device. The tumor was located near the subclavian vein, and we were able to remove the tumor from the safety of these major vessels (Figure 2A). After that, partial resection—including that of the tumor on the right lung apex—was performed through a transmanubrial incision, and the tumor was diagnosed as a non-small cell carcinoma of the lung by intraoperative frozen section analysis. We decided to perform a right upper lobectomy. While waiting for the analysis of the frozen section of the right lung tumor, the left apex tumor was resected with VATS using 3 port incisions while in the supine position without postural change; only the operating table was tilted with the left side up. The ports were located in the third and fourth intercostal spaces on the midclavicular line and the fifth intercostal space on the anterior axillary line (Figure 2B). The left lung apex was extensively adhered to the parietal pleura but could be easily detached by VATS. The left lung tumor in the bulla was palpable, and partial resection was performed using an endostapler (Figure 2C). Then, the patient shifted to the left lateral position, 2 ports were added on the fifth and seventh intercostal spaces of the posterior axillary line, and we performed right upper lobectomy and lymphadenectomy through 4 ports using VATS (Figure 2D). Pathological findings revealed that the right lung tumor had epithelial and spindle cell components. The tumor was diagnosed as pleomorphic carcinoma (pT2bN0M0) and completely resected (Figure 3A). The tumor had no lymph node metastases but showed vascular invasion (V1) and pleural invasion (pl1). The left lung tumor had large atypical cells without cell differentiation to adenocarcinoma or squamous cell carcinoma and was diagnosed as large cell carcinoma (pT1aNXM0) (Figure 3B). The left chest tube was removed on the first day after surgery and the right chest tube was removed on the second day after surgery. The patient continued rehabilitation and was discharged from our hospital 12 days after surgery with no major postoperative complications. After confirming the diagnosis, we suggested a left upper lung lobectomy and lymphadenectomy, but the patient declined. He remains healthy while continuing to work as a sushi chef and is recurrence-free 7 years after the surgery.
All procedures performed in this study were in accordance with the ethical standards of the institutional and national research committee(s) and with the Helsinki Declaration (as revised in 2013). Written informed consent was obtained from the patient for publication of this case report and accompanying images. A copy of the written consent is available for review by the editorial office of this journal.
Discussion
Selecting an appropriate surgical approach for SST is difficult as surgery must be carefully performed to avoid damage to important adjacent anatomical structures, such as the subclavian and jugular vessels, phrenic nerve, and trunks of the brachial plexus (3). To resect anterior SST, we followed the TMA first described by Grunenwald and Spaggiari (4). It is a useful and safe approach because it enables good visualization of important structures without altering shoulder mobility. Even if the tumor cannot be detached from the major vessel, TMA can facilitate resection of the vessel and its replacement with an artificial blood vessel. In addition, a combined approach involving TMA and VATS is a useful and minimally invasive method for the resection of SST. Table 1 shows case reports of TMA combined with VATS for lung cancer, as searched from PubMed (1,5-9). Two patients underwent surgery only in the supine position. The mean length of hospital stay was 12.7 days and the mean disease-free interval was 35.6 months. Rosso et al. reported that performing a VATS observation before the anterior surgical approach would help exclude previously undetected pleural dissemination and precisely define the tumor location (1). Kayawake et al. reported that viewing not only from the neck side, but also from intrathoracic side, helps identify important anatomical structures (2).
Table 1
| First author | Age (years)/sex | Side | Pathology | C-stage | Approach | Patient position | Extended resection | P-stage | LOS (day) | complications | Outcome |
|---|---|---|---|---|---|---|---|---|---|---|---|
| Truin | 60/F | R | NSCLC | cT3N0M0 | Apex→VATS | Supine→lateral | 1st rib + T1 root + subclavian vein | ypT0N0M0 | 7 | Right aim mild edema | NA |
| Nakajima | 59/M | L | NSCLC | cT3N0M0 | Apex→VATS | Supine | 1st rib + T1 root + anterior scalene muscle | ypT0N0M0 | NA | Atelectasis phrenic nerve paralysis | NA |
| Shikuma | 59/M | L | NSCLC | cT3N0M0 | Apex→VATS | Supine→lateral | None | ypT3N0M0 | NA | NA | 24-month alive |
| Yokoyama | 79/M | R | Pleo | cT3N0M0 | VATS→Apex | Lateral→supine | 1st +2nd ribs | pT3N0M0 | 18 | NA | 48-month alive |
| 51/M | L | NSCLC | cT4N0M0 | VATS→Apex | Lateral→supine | 1st rib+T1 root + subclavian vein | ypT3N0M0 | 17 | NA | 16-month alive | |
| Rosso | 50/F | R | Ad | cT3N0M0 | VATS→Apex | Supine | 1st +2nd ribs | ypT0N0M0 | 9 | Hyperpyrexia | 6-month alive |
| Oka | 71/M | L | Sq | cT3N0M0 | Apex→VATS | Supine→lateral | 1st +2nd ribs | pT3N0M0 | 13 | None | NA |
| Present case | 68/M | R | Pleo | cT3N0M0 | Apex→VATS | Supine→lateral | Left lung apex tumor | pT2bN0M0 | 12 | None | 84-month alive |
NSCLC, non-small cell carcinoma; Pleo, pleomorphic carcinoma; Ad, adenocarcinoma; Sq, squamous cell carcinoma; LOS, length of stay; TMA, transmanubrial approach; VATS, video-assisted thoracoscopic surgery.
In our case, the surgery commenced with VATS observation to locate the tumor and to exclude pleural dissemination. First, we evaluated tumor resectability using 3 ports in VATS. If the tumor could be resected, TMA would not be required and conventional VATS lobectomy could be performed. In the supine position, we were able to remove the anterior SST from the subclavian vessels with TMA, and also resect the left upper tumor with VATS. Without changing the posture, we were able to avoid the time-consuming maneuvers required for patient repositioning and the risk of endotracheal tube displacement.
There are several technical tips regarding resection of the left upper tumor with VATS. The operating table was tilted upwards on the left side to make it more convenient for the surgeons to use the forceps. The ports were located in front of the normal position as the patient lay in the supine position. Opting for thoracoscopic surgery ensured a good field of view up to the apex of the lungs even if the ports were located on the midclavicular line. Fortunately, we could locate the left lung tumor by VATS; however, if the location of the tumor is unclear, it may be possible to locate the tumor by inserting a port or hand from the wound of TMA, such as in hand-assisted thoracoscopic surgery.
Pulmonary pleomorphic carcinoma is a rare malignant tumor. Previous reports noted that the overall median postoperative survival was 8–10 months for patients with pulmonary pleomorphic carcinoma (10,11). Despite developing high-grade double primary lung carcinoma, the patient in our case remains healthy and recurrence-free 7 years after the surgical treatment, indicating that our surgical approach to bilateral apex tumors is potentially effective and safe for the complete resection of bilateral lung tumors.
Acknowledgments
We would like to thank Editage (www.editage.com) for English language editing.
Funding: None.
Footnote
Reporting Checklist: The authors have completed the CARE reporting checklist. Available at https://asj.amegroups.com/article/view/10.21037/asj-21-13/rc
Peer Review File: Available at https://asj.amegroups.com/article/view/10.21037/asj-21-13/prf
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at https://asj.amegroups.com/article/view/10.21037/asj-21-13/coif). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. All procedures performed in this study were in accordance with the ethical standards of the institutional and/or national research committee(s) and with the Helsinki Declaration (as revised in 2013). Written informed consent was obtained from the patient for publication of this case report and accompanying images. A copy of the written consent is available for review by the editorial office of this journal.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Rosso L, Palleschi A, Mendogni P, et al. Video-assisted pulmonary lobectomy combined with transmanubrial approach for anterior Pancoast tumor resection: case report. J Cardiothorac Surg 2016;11:65. [Crossref] [PubMed]
- Kayawake H, Chen-Yoshikawa TF, Date H. Dual approach for large mediastinal tumors in the thoracic outlet: transmanubrial osteomuscular sparing approach and video-assisted thoracoscopic surgery. J Cardiothorac Surg 2019;14:42. [Crossref] [PubMed]
- Marulli G, Battistella L, Mammana M, et al. Superior sulcus tumors (Pancoast tumors). Ann Transl Med 2016;4:239. [Crossref] [PubMed]
- Grunenwald D, Spaggiari L. Transmanubrial osteomuscular sparing approach for apical chest tumors. Ann Thorac Surg 1997;63:563-6. [Crossref] [PubMed]
- Truin W, Siebenga J, Belgers E, et al. The role of video-assisted thoracic surgery in the surgical treatment of superior sulcus tumors. Interact Cardiovasc Thorac Surg 2010;11:512-4. [Crossref] [PubMed]
- Nakajima T, Watanabe A, Nakazawa J, et al. Transmanubrial approach with video-assisted thoracoscopic surgery for left superior sulcus tumour with dense adhesion after replacement of descending thoracic aorta. Interact Cardiovasc Thorac Surg 2012;14:906-8. [Crossref] [PubMed]
- Shikuma K, Miyahara R, Osako T. Transmanubrial approach combined with video-assisted approach for superior sulcus tumors. Ann Thorac Surg 2012;94:e29-30. [Crossref] [PubMed]
- Yokoyama Y, Chen F, Aoyama A, et al. Combined operative technique with anterior surgical approach and video-assisted thoracoscopic surgical lobectomy for anterior superior sulcus tumours. Interact Cardiovasc Thorac Surg 2014;19:864-6. [Crossref] [PubMed]
- Oka S, Ono K, Kajiyam K, et al. A minimally invasive and safe surgical approach to resect anterior superior sulcus tumors. Int J Surg Case Rep 2020;68:148-50. [Crossref] [PubMed]
- Fishback NF, Travis WD, Moran CA, et al. Pleomorphic (spindle/giant cell) carcinoma of the lung. A clinicopathologic correlation of 78 cases. Cancer 1994;73:2936-45. [Crossref] [PubMed]
- Raveglia F, Mezzetti M, Panigalli T, et al. Personal experience in surgical management of pulmonary pleomorphic carcinoma. Ann Thorac Surg 2004;78:1742-7. [Crossref] [PubMed]
Cite this article as: Kumeda H, Hamanaka K, Agatsuma H, Yoshida K, Shimizu K. Transmanubrial approach with thoracoscopic surgery for bilateral lung cancer: a case report. AME Surg J 2021;1:29.


