
Successful right lower bilobectomy for endobronchial carcinosarcoma rapidly occluding the trachea: a case report
Introduction
Endobronchial carcinosarcoma is an extremely rare type of malignant tumor (1). Because these polypoidal lesions present necrotic tissue without invasion of the bronchus mucosa, radical lung function-preserving resection may be possible. It should be noted that careful endobronchial examination is required to check for endobronchial invasion before curative resection. We present the following case in accordance with the CARE reporting checklist (available at https://asj.amegroups.com/article/view/10.21037/asj-21-109/rc).
Case presentation
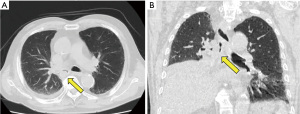
A 73-year-old man with dyspnea upon exercise was investigated by computed tomography (CT), and atelectasis of the right middle and lower lobe, as well as a polypoid tumor originating from the lower lobe and extending into the right main bronchus, were identified (Figure 1A,1B). Two weeks after the CT examination, diagnostic bronchoscopy was undertaken under local anesthesia at the referral hospital, which revealed that the whitish polypoid tumor contained only necrotic tissue. In the second bronchoscopy performed 2 weeks later, the patient presented with acute respiratory failure because the tumor had already extended beyond the carina to occlude the trachea (Figure 2A). He required urgent left mainstem bronchial intubation and was transferred to our hospital with mechanical ventilation support for further treatment.

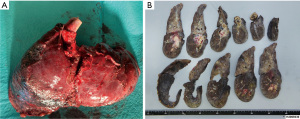
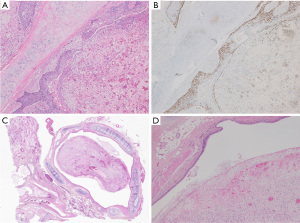
On arrival, the tracheal tube in the left mainstem bronchus was pulled back to the trachea under careful bronchoscopic observation. Because the tumor appeared to grow like a polyp without invading the mucosa of the right main bronchus, we decided to debulk the tumor by flexible bronchoscopy under extracorporeal membrane oxygenation (ECMO) support because of unstable oxygenation. To avoid bleeding, the activated clotting time was maintained at 150–180 seconds. Using the snare technique, we successfully removed a polypoid tumor of approximately 3 cm in size, which allowed stable oxygenation due to recovery of the ventilation of the right upper lobe and withdrawal from ECMO support (Figure 2B,2C). Because positron emission tomography-CT suggested that there was no evidence of distant metastasis, a right lower bilobectomy was planned 1 week after the debulking without definitive diagnosis. A right posterolateral thoracotomy was performed. Intraoperative findings showed an edematous lung with no sign of tumor dissemination. Because the middle lobe was invaded by the tumor, which developed extrabronchially beyond the major fissure and presented pneumonia, we decided to perform a bilobectomy. After the bronchus intermedium was exposed, the bronchial wall was carefully incised with a sharp scalpel to avoid cutting into the endobronchial polyp. After peeling off the circumference wall of the bronchus intermedius, the whitish polyp originating from the lower lobe was successfully extracted en block from the right main bronchus (Video 1). After a negative bronchial margin was confirmed on frozen sections, the bronchial stump was sutured with interrupted 4-0 PDS stitches and covered with a pedicled pericardial fat pad. The postoperative course was uneventful. Pathological examination showed that the tumor (10.5×3.8×3.2 cm3) originated from the proximal portion of the lower bronchus and extended to the lung parenchyma extrabronchially around the inlet of B8–10 and the middle lobe (Figure 3A,3B), but the bronchus intermedium was not invaded. The tumor comprised chondrosarcoma and squamous cell carcinoma, and it was diagnosed as endobronchial carcinosarcoma (pT4N1M0) (Figure 4A,4B). The tumor that presented endobronchial extension comprised only the sarcomatous component, and the surface of the whitish polyp was covered by necrotic tissue of 0.5 mm in thickness (Figure 4C,4D). The patient received adjuvant chemotherapy with cisplatin and vinorelbine and had developed no recurrence at 14 months after surgery. All procedures performed in this study were in accordance with the ethical standards of the institutional and/or national research committee(s) and with the Helsinki Declaration (as revised in 2013). Written informed consent was obtained from the patient for publication of this case report and accompanying images. A copy of the written consent is available for review by the editorial office of this journal.
Discussion
Pulmonary carcinosarcoma is a rare subtype of lung cancer, accounting for 0.2–0.3% of cases, and comprises both carcinomatous and sarcomatous components; the former contains an element of squamous cell carcinoma or epidermoid, and the latter contains fibro- or spindle-cell sarcoma (1). It is divided into endobronchial and peripheral types, and the endobronchial type has a characteristic appearance presenting as bronchial polyps. This tumor type extends to the proximal bronchus without invasion of the adjoining bronchial mucosa in a polypoid fashion, and the surface of the polyp often shows ulceration and necrosis, as in our case. Ludwigsen et al. reported that the left main bronchus was totally obstructed by carcinosarcoma originating in the upper lobe bronchus and protruding into the lower lobe bronchus similar to a polypoid tumor, which presented intractable hemorrhage after multiple biopsies (2). Furthermore, Kakos et al. described that the usual preoperative diagnostic methods were unrewarding because the area accessible to the transbronchial biopsy was covered with necrotic tissue (3).
In our case, flexible bronchoscopic debulking using the snare technique provided stable oxygenation due to recovery of ventilation of the right upper lobe. However, the bronchus intermedium could not be fully observed because the lumen was tightly occupied by the solid polyp, and secondary bronchial obstruction hampered sufficient preoperative endobronchial evaluation. Because rigid bronchoscopy has proven to be an excellent tool to control central airway obstruction due to neoplastic or non-neoplastic disease, to conduct more lung parenchymal-saving procedures including lower sleeve lobectomy, rigid bronchoscopy might have been performed to obtain a better tissue sample. Endobronchial carcinosarcoma can mislead the preoperative staging of the disease to a more advanced stage. It should be noted that careful endobronchial examination is required to check for endobronchial invasion before curative resection.
Regarding the outcome of the surgical treatment, the prognosis of endobronchial carcinosarcoma is generally poor. The 1-year survival rate is 42% and the 5-year survival rate is 21.3% (2-6). Koss et al. reported that the most important predictor of poor prognosis was a tumor size larger than 6 cm (1). While several reports described the effectiveness of chemotherapy for carcinosarcoma, surgical resection should be considered not only as a radical treatment prior to distant metastases but also as a palliative treatment before fatal tracheal obstruction.
Conclusions
In conclusion, polypoidal lesions of endobronchial carcinosarcoma present necrotic tissue without invasion of the bronchus mucosa. Because radical lung function-preserving resection may be possible, careful endobronchial examination is required to check for endobronchial invasion before curative resection.
Acknowledgments
We thank H. Nikki March, PhD, Edanz (https://www.jp.edanz.com/ac) for editing a draft of this manuscript.
Funding: None.
Footnote
Reporting Checklist: The authors have completed the CARE reporting checklist. Available at https://asj.amegroups.com/article/view/10.21037/asj-21-109/rc
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at https://asj.amegroups.com/article/view/10.21037/asj-21-109/coif). YY serves as an unpaid editorial board member of AME Surgical Journal from January 2021 to December 2024. The other authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. All procedures performed in this study were in accordance with the ethical standards of the institutional and/or national research committee(s) and with the Helsinki Declaration (as revised in 2013). Written informed consent was obtained from the patient. A copy of the written consent is available for review by the editorial office of this journal.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Koss MN, Hochholzer L, Frommelt RA. Carcinosarcomas of the lung: a clinicopathologic study of 66 patients. Am J Surg Pathol 1999;23:1514-26. [Crossref] [PubMed]
- Ludwigsen E. Endobronchial carcinosarcoma. A case with osteosarcoma of pulmonary invasive part, and a review with respect to prognosis. Virchows Arch A Pathol Anat Histol 1977;373:293-302. [Crossref] [PubMed]
- Kakos GS, Williams TE Jr, Assor D, et al. Pulmonary carcinosarcoma. Etiologic, therapeutic, and prognostic considerations. J Thorac Cardiovasc Surg 1971;61:777-83.
- Sun L, Dai J, Wang X, et al. Pulmonary carcinosarcoma: analysis from the Surveillance, Epidemiology and End Results database. Interact Cardiovasc Thorac Surg 2020;30:4-10. [Crossref] [PubMed]
- Park SJ, Choo JY, Lee KY, et al. Usefulness of Digital Tomosynthesis for the Detection of Airway Obstruction: A Case Report of Bronchial Carcinosarcoma. Cancer Res Treat 2015;47:544-8. [Crossref] [PubMed]
- Huwer H, Kalweit G, Straub U, et al. Pulmonary carcinosarcoma: diagnostic problems and determinants of the prognosis. Eur J Cardiothorac Surg 1996;10:403-7. [Crossref] [PubMed]
Cite this article as: Yutaka Y, Nagata S, Sugimoto A, Date H. Successful right lower bilobectomy for endobronchial carcinosarcoma rapidly occluding the trachea: a case report. AME Surg J 2023;3:19.


